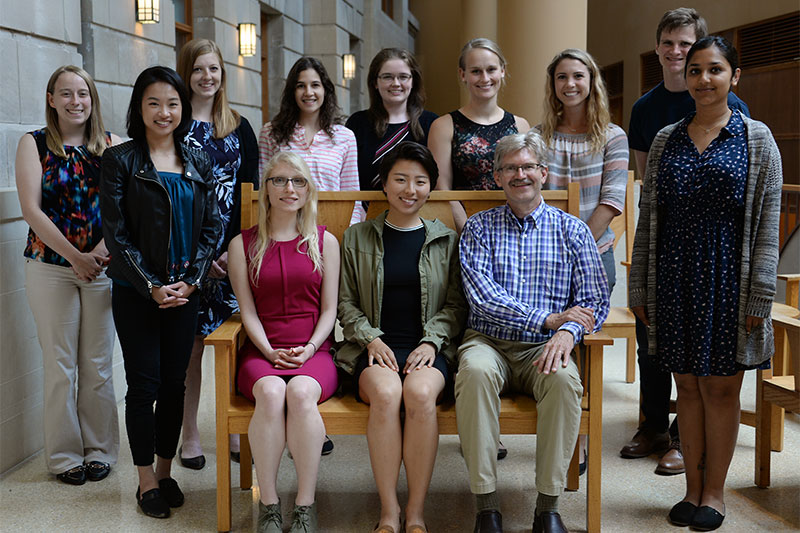
This year’s Summer Student Research and Clinical Assistantship participants. Back row, from left: Beth Klein, Thao Nguyen, Kathryn Henschel, Ninah Divine, Brooke Olson, Jillian Hess, Payden White, Matthew Goblirsch, Nivi Nair. Seated, from left: Lenka Craigova, Yanzi Jiang, Jonathan Temte, MD, PhD. (Not pictured: Mariana Nino de Guzman Ramirez and Noah John Borchardt.)
Every summer, the UW Department of Family Medicine and Community Health (DFMCH) welcomes medical students to participate in people-oriented, clinically relevant, hands-on research projects through its eight-week Summer Student Research and Clinical Assistantship (SSCRA).
Led by DFMCH Professor Jonathan Temte, MD, PhD, the program gives students the opportunity to see patients in a variety of settings and learn important research skills. It also helps DFMCH faculty advance research projects in family medicine and community health.
For example, last year, SSCRA student Danika Johnson worked with David Hahn, MD, a senior scientist in the DFMCH’s Wisconsin Research and Education Network, to survey patients with coughs at five Wisconsin clinics and identify which ones used menthol cough drops. That work resulted in a paper (published in the Journal of the American Board of Family Medicine) showing that excessive use of menthol cough drops could actually increase coughs.
This year, 13 SSCRA students joined Dr. Temte and DFMCH faculty on a new set of research projects. Learn more about them below.
Project Spotlight: Factors which Affect the Decision of Family Physicians that Enter Practice in Underserved Communities
In her project, SMPH student Lenka Craigova (mentors: Ildi Martonffy, MD; John J. Frey III, MD; Justin Sena; Stephanie Sippl; William Buckingham, PhD), carried out structured interviews with 50 randomly selected graduates of DFMCH-sponsored residency programs to identify reasons why they did or did not choose to enter practice in an underserved community.
Her interview questions focused on the following themes: integration within the community; scope and structure of practice (including relief coverage and control over working hours); experiences during medical education; financial burden; the physicians’ formative years (i.e., a rural upbringing); family influences; and deterrents and ongoing challenges.
The team hopes to use this qualitative data to inform policies that may affect career choices for future family physicians.
Project Spotlight: Prolotherapy, Osteopathic Manipulation, and Platelet Rich Plasma For Pain and Disability in a Patient with Hypermobile Ehlers-Danlos Syndrome
In this project, SMPH student Jillian Hess (mentors: David Rabago, MD, Mike Weber, MD, and Bobby Nourani, DO) used a mixed-methods approach of validated outcome questionnaires, chart review and qualitative interview to develop a case report assessing the effects of prolotherapy, osteopathic manipulative treatment and platelet-rich plasma injection for a patient with hypermobile Ehlers Danlos Syndrome (hEDS).
The report revealed that from baseline to 18 months post treatment, the patient’s pain and disability decreased, and quality of life increased. It provides feedback on clinical practice guidelines; offers a framework for early signals of effectiveness, adverse events, and cost; and adds to the literature on the hEDS population.
Project Spotlight: Role of Exposure to Nature in Mitigating Dysphoria related to Global Climate Change
In this project, SMPH student Ninah Divine (mentor: Jonathan Temte, MD, PhD), surveyed 421 English-speaking adult patients at the DFMCH’s four residency clinics to gain insight on the relationship between patient attitudes toward climate change, dysphoria and exposure to nature.
Of those patients, 22.8 percent scored positive for dysphoria; on average, they spent 3.3 days per week in natural settings. Greater exposure to nature was associated with decreased dysphoria, but increased anxiety about climate change. Climate change may hinder positive effects of exposure to nature by increasing anxiety about global warming and extreme weather.
More Diverse Research Projects
In addition to their work on the projects highlighted above, this year’s SSCRA students:
- Helped develop policies and protocols for Madison Area Care for the Homeless (MACH) OneHealth, an outreach program focused on providing direct medical care on the streets for unsheltered homeless in Madison;
- Gathered clinician, health care staff and community input for a proposed pilot project to integrate community health workers into the DFMCH’s family medicine clinics;
- Assisted a research team on a project to pilot a screening protocol for opioid risk among patients at Wisconsin trauma centers;
- Collaborated with the Madison Addiction Recovery Initiative (MARI) team to collect data and learn how city-wide, interdisciplinary initiatives can impact public health and treatment outcomes in individuals with addiction;
- Evaluated data from an earlier survey of providers at Access Community Health Centers Wingra Family Medical Center to assess their knowledge, attitudes and prescribing practices regarding emergency contraception (EC), and increase their awareness of current guidelines for EC prescribing;
- Participated in a diabetes treatment program in San Lucas Tolimán, Guatemala, that uses local community health workers and a smartphone application to provide clinical guidance;
- Helped developed a case series on the outcomes of switching diabetic patients in a Madison nursing home from insulin to DPP-4 inhibitors;
- Collected and analyzed data and prepared a draft manuscript on the incidence of pharyngeal gonorrhea and chlamydia at a high-risk STD clinic in Milwaukee; and
- Evaluated and proposed strategies to improve communication between patients treated for tuberculosis, Zero TB staff, and healthcare providers at Tibetan Delek Hospital in Dharamshala, India.
To learn more about the SSCRA program, visit the program page or contact Dr. Temte.
Published: July 2018
